Patient 5: Wong Wei Hong
Age: 67 years old
Sex: Male
Complaints: Fever, chills, bladder distension
(bladder stretching); on indwelling catheter
(a catheter inserted in the urethra to continuously empty the bladder into a drainage collector)
Diagnosis: Urinary Tract Infection
Antibiotic treatment: Nil
Indwelling catheters
Indwelling catheters avoid distension by emptying the bladder continuously into a bedside drainage collector. Individuals with indwelling catheters are encouraged to maintain a high fluid intake in order to prevent bacteria from accumulating and growing in the urine.
1Urinary Tract Infection (UTI)It is a condition where one or more structures in the urinary tract become infected after bacteria overcome its strong natural defenses.
There are three main types of UTI.
-
Urethritis, caused by bacteria that infects the urethra
(the short tube that delivers urine from the bladder to the outside of the body).
-
Cystitis, caused by bacteria that infects the bladder.
-
Pyelonephritis, caused by bacteria that infect the kidneys. It is more serious.
2UTI can also be categorized into
complicated or uncomplicated.
Uncomplicated – Associated with bacterial infection, usually
Escherichia coli (
E.coli). Affect women more often than men.
Complicated – Occur as often in men as in women. Associated with bacterial infection but usually caused by some anatomical or structural abnormality, such as
catheter use in hospital, bladder and kidney dysfunction or kidney transplant. Recurrences occur in up to 50% to 60% of patients with complicated UTI if the underlying structural or anatomical abnormalities are not corrected.
3UTI in this patient should be due to the presence of the catheter in the urethra.
Complicated UTIs may develop because of any one of a number of physical problems and affect any gender and age group. The common feature in most complicated UTIs is the inability of the urinary tract to clear out bacteria because of a physical condition that causes obstruction to the flow of urine or problems that hinder treatment success.
3For Catheterized and hospitalized patients- Symptoms may be atypical or may be attributed to other disease processes, and no reliable colony count cutoff defines significant bacteriuria. Low-level (100-1000 colony-forming units [CFU] per mL) colonization can progress to high-level (>100,000 CFU/mL) bacteriuria within 3 days in 96% of catheterized patients who are cultured on subsequent days (and not treated with antimicrobials). Thus, most experts agree that growth of more than 100 CFU/mL of a predominant pathogen represents catheter-related UTI.
-Polymicrobial bladder infections are not uncommon in catheterized patients, and nonpathogenic organisms can be significant in catheterized patients.
3Organisms in Complicated Infections
Complicated UTIs, which are related to physical or structural conditions, are usually caused by a wider range of organism.
E. coli is still the most common organism, but others have also been detected, including the following:
Other intestinal bacteria, including
Klebsiella pneumoniae (K.pneumoniae), Proteus mirabilis (P.mirabilis) , and Citrobacter.
Others include
Pseudomonas aeruginosa (P.aeruginosa), Enterobacter, and
Serratia species, gram-positive organisms, including
Enterococcus species, and
S. saprophyticus .
3In this particular case, the urine specimen should be sent for a urine culture, a test to identify the exact type of bacteria causing the infection.
Urine Culture and Susceptibility TestingThe presence of a single type of bacteria growing at high colony counts (>10,000 colony forming units (CFU)/ml) is considered a positive urine culture and indicates an infection. Any bacterial infection may be serious and can spread to other areas of the body if not treated.
4Susceptibility Testing tests for the likelihood that a particular antimicrobial will be effective in killing or sufficiently inhibiting the growth of the specific pathogens that is causing the infection. It measures whether or not the microorganism can grow when it is exposed to a variety of antimicrobials in a laboratory test. A culture of the infected area must be done to obtain the organism for identification before susceptibility testing is done. The culture involves incubating a sample at body temperature in a nutrient- rich environment. This process promotes the growth of any microorganisms present in the sample. Urine samples are usually sterile; they will show little or no growth unless a pathogenic microorganism is present.
The pathogens are isolated and identified using biochemical and enzymatic tests. Each type of bacteria that may be clinically significant in the specimen (a pathogen) is tested individually to determine the ability of antimicrobials to inhibit its growth. Susceptibility testing is performed by growing the pure bacterial isolate in the presence of varying concentrations of several antimicrobials and then examining the amount of growth to determine which antimicrobials at which concentrations inhibit the growth of the bacteria. Results of the testing are reported as “Susceptible” (likely, but not guaranteed to inhibit the pathogenic microorganism), “Intermediate” (may be effective at a higher than normal concentration), and “Resistant” (not effective at inhibiting the growth of the organism).
5Gram StainThis is a staining procedure that can be done after a urine culture is done to make bacteria visible through a microscope. The bacteria are categorized
gram-positive and gram-negative.
Bacteria that turn pink from staining are called gram-negative.
Those that turn blue are called gram-positive.
E.coli is gram negative and the most common cause of UTIs.
6Antibiotics for Catheter-Induced Infections
A major problem in treating catheter-related UTIs is that the organisms involved are constantly changing and that there might be multiple species of bacteria present at the same time, therefore an antibiotic that is effective against a wide variety of microorganisms is usually recommended. These medications include those in the fluoroquinolone group and drug combinations such as ampicillin plus gentamicin or imipenem plus cilastatin.
7Suspected organisms: E.coli, Stahylococcus aureus (S.aureus), P.mirabilis, K.pneumoniae and
P.aeruginosa.E.coli-Gram-negative, rod-shaped bacterium
-Propelled by long, rapidly rotating flagella.8
-Usually infect urinary tract
-Accounts for more than 90% of all uncomplicated UTIs.
-Recurrence rate is 44% over 12 months.
-Caused by uropathogenic strains of E coli.
-Facultatively anaerobic
-Grow on MacConkey plate
-Catalase Positive and Oxidase Negative
-The pathogenesis is using an adherence factor called fimbriae or pili, which binds to the P blood group antigen. These fimbriae mediate the attachment of
E.coli to uroepithelial cells. Thus, patients with intestinal carriage of
E.coli containing P fimbriae are at greater risk of developing UTI compared with the general population.
-Complicated UTI and pyelonephritis are observed in elderly patients with structural abnormalities or obstruction such as prostatic hypertrophy, neurogenic bladders, or in the presence of urinary catheters.
-Bacteremia (bacteria in the blood) due to
E.coli is usually associated with UTIs, especially in cases of urinary obstruction of any cause. The systemic reaction to endotoxin (cytokines) or lipopolysaccharides can lead to disseminated intravascular coagulation and death.
E.coli is a leading cause of nosocomial bacteremia (infections that result of treatment in a hospital) from a GI or genitourinary source.
9S.aureus-Gram-positive, cluster-forming coccus
-nonmotile, nonsporeforming facultative anaerobe
-fermentation of glucose produces mainly lactic acid
-ferments mannitol (distinguishes from
S.epidermidis)
-catalase positive
-coagulase positive
-Causes a variety of suppurative (pus-forming) infections and toxinoses in humans. It causes superficial skin lesions such as boils, more serious infections such as pneumonia nd urinary tract infections; and deep-seated infections, such as osteomyelitis and endocarditis.
-A major cause of nosocomial (hospital acquired) infection of surgical wounds and infections associated with indwelling medical devices.
-Causes food poisoning by releasing enterotoxins into food, and toxic shock syndrome by release of superantigens into the blood stream.
-Hospital strains of
S.aureus are usually resistant to a variety of different antibiotics. The term MRSA refers to Methicillin resistant
S.aureus. Methicillin resistance is widespread and most methicillin-resistant strains are also multiply resistant.
-
S.aureus exhibits resistance to antiseptics and disinfectants, aiding its survival in the hospital environment.
-These organisms are uniformly resistant to penicillins and cephalosporins. Usually Vancomycin are used.
10P.aeruginosa-Rare bacterial agents, most often detected in hospital-acquired UTIs.
11
-Gram-negative,aerobic, rod shaped bacterium
-Secretes a variety of pigments, including pyocyanin (blue-green), fluorescein (yellow-green and fluorescent) and pyorubin (red-brown). Pseudomonas Agar P (King A media) can enhance pyocyanin and pyorubin production while Pseudomonas Agar F (King B media) can enhance fluorescein production.
-Pearlescent appearance and grape-like odour.
-Can grow at 42°C.
-Naturally resistant to a large range antibiotics. The antibiotics that are useful in eliminating
P.aeruginosa include aminoglycosides, quinolones, cephalosporins and carbapenems.
12-Pseudomonal infections of the urinary tract usually are hospital-acquired and iatrogenic, related to catheterization, instrumentation, and surgery.
13
P.mirabilias
-Gram-negative, facultatively anaerobic bacterium
-Swarming, motility and urease activity.
-Infection gives an alkaline urine sample.
-Inability to metabolize lactose, like on a MacConkey agar plate.
-Generally susceptible to most antibiotics apart from tetracycline.
-Utilize urea and citrate, produce Hydrogen Sulfide gas and forms clear films on growth media.
-Indole Negative
-Catalase Positive and Oxidase Negative14K.pneumoniae
-Gram-negative, facultatively anaerobic, rod-shaped bacterium
-Non-motile, encapsulated
-Lactose-fermenting
-Indole Negative
-Catalase Positive and Oxidase Negative
-Commonly implicated in hospital acquired urinary tract and wound infections.
-Possesses a chromosomal class A beta-lactamase, giving rise to an inherent resistance to ampicillin. Many strains have acquired an extended spectrum beta lactamase (ESBL) with additional resistance to carbenicillin, ampicillin, quinolones.15
Bichemical Tests to distinguish the suspected organisms:
For Gram Positive Cocci, Catalase test can be done. This is by adding Hydrogen Peroxide to the isolated colonies. A Positive result is indicated by the presence of bubbles. If result is positive, the pathogen can be said to be Staphylococcus.
The next test that can be done is the Coagulase test. S.aureus produce coagulase which clots citrated plasma which then binds to prothrombin and initiate fibrin polymerization. S.aureus will produce a clumping factor on its surface and fibrin adhere to these factors and causes agglutination reaction. Therefore, a positive result, judged by an agglutination reaction, indicates that the pathogen present is S.aureus.
For Gram Negative Bacilli, Oxidase test can be done. The principle of this test is using the presence of cytochrome oxidase activity and transferring electrons to oxygen. Bacteria will oxidize the oxidase disk and turn it purple in colour which indicates a positive result. If this is the case, the pathogens can be grown on a Mueller Hinton agar plate and if it produce green colonies, the pathogen is P.aeruginosa. If the oxidase test remain colourless, the pathogens can be grown on a CLED agar plate. CLED will prevent swarming of proteus and it differentiates between Lactose fermentor and Non-lactose fermentator. Lactose Fermentor will produce yellow colonies on CLED agar. If this is the case, Indole test can be done to identify E.coli whereby indole will react with aldehyde group to produce a positive result which is pink/purple in colour. Non fermentor will be blue in colour on CLED agar.
1. http://www.healthatoz.com/healthatoz/Atoz/common/standard/transform.jsp?requestURI=/healthatoz/Atoz/ency/neurogenic_bladder.jsp
2. http://www.kidshealth.org/teen/infections/common/uti.html
3. http://www.reutershealth.com/wellconnected/doc36.html
4. http://www.labtestsonline.org/understanding/analytes/urine_culture/test.html
5.http://www.labtestsonline.org/understanding/analytes/susceptibility/glance-2.html
6.http://www.hmh.net/adam/patientreports/000036.htm
7.http://www.hmh.net/adam/patientreports/000036.htm
8.http://education.yahoo.com/reference/encyclopedia/entry/Escheri
9.http://www.emedicine.com/med/topic734.htm
10. www.textbookofbacteriology.net/staph.html
11. http://www.reutershealth.com/wellconnected/doc36.html
12. http://en.wikipedia.org/wiki/Pseudomonas_aeruginosa
13. http://www.emedicine.com/MED/topic1943.htm
14. http://en.wikipedia.org/wiki/Proteus_mirabilis
15. http://en.wikipedia.org/wiki/Klebsiella
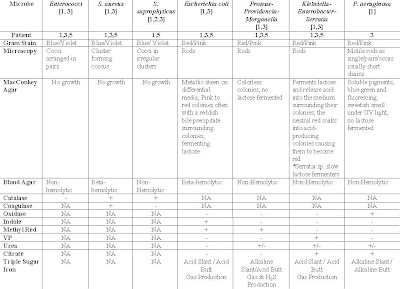 Table 1: Suspected Organisms, Relevant tests and expected results of tests for respective patients diagnose with UTI
Table 1: Suspected Organisms, Relevant tests and expected results of tests for respective patients diagnose with UTI






 jade.ccccd.edu/mweis/.../media_SD_list_page.htm
jade.ccccd.edu/mweis/.../media_SD_list_page.htm

 Oxidase
Oxidase












